Pressure ulcer prevention
Last edited: 20/06/2023
Alternative formats
This leaflet is available in:
How to help prevent pressure ulcers. If there is anything else you need to know, please speak to your healthcare professional.
What is a pressure ulcer?
A pressure ulcer is localised damage that occurs to the skin and/or underlying tissue, usually over a bony prominence (or related to a medical or other device). It is caused by unrelieved pressure, shearing, or a combination of these.
Pressure ulcers range from mild damage (redness and breaks in the skin) to deeper damage (dark red and purple; black hard patches that can develop into bigger wounds).
Causes of pressure ulcers
Pressure
- Concentration of body weight over one area for a period of time.
Shearing
- Sliding or slumping down the bed and/or chair.
- Sitting on an inappropriate sized chair (too wide or small, too high or low).
- Sliding down the bed and pushing yourself back up.
- Damage caused by poor moving methods from bed to chair, or in-bed repositioning.
- Rubbing and/or massaging.
- Ill-fitting clothing and/or shoes.
- Straps and/or hoist etc.
If you are unable to visually see the areas please report any new sensations, (soreness, pain, numbness) to your healthcare professional.
Are you at risk?
You may be at risk of developing pressure ulcers for a number of reasons, including the following:
- cannot or unable to move very well
- sitting or wheelchair use for long periods
- poor blood circulation
- spinal cord injury resulting in loss of sensation
- diabetes, neurological diseases, stroke, heart disease and lung disease
- if you smoke
- if you suffer from incontinence
- if you perspire or sweat
- previous wounds to any of the common locations (shown on page two)
- have lots of skin folds
- inadequate diet or fluid intake
- underweight or overweight
- very ill or have had complicated surgery
- dry, oedematous or poor skin condition.
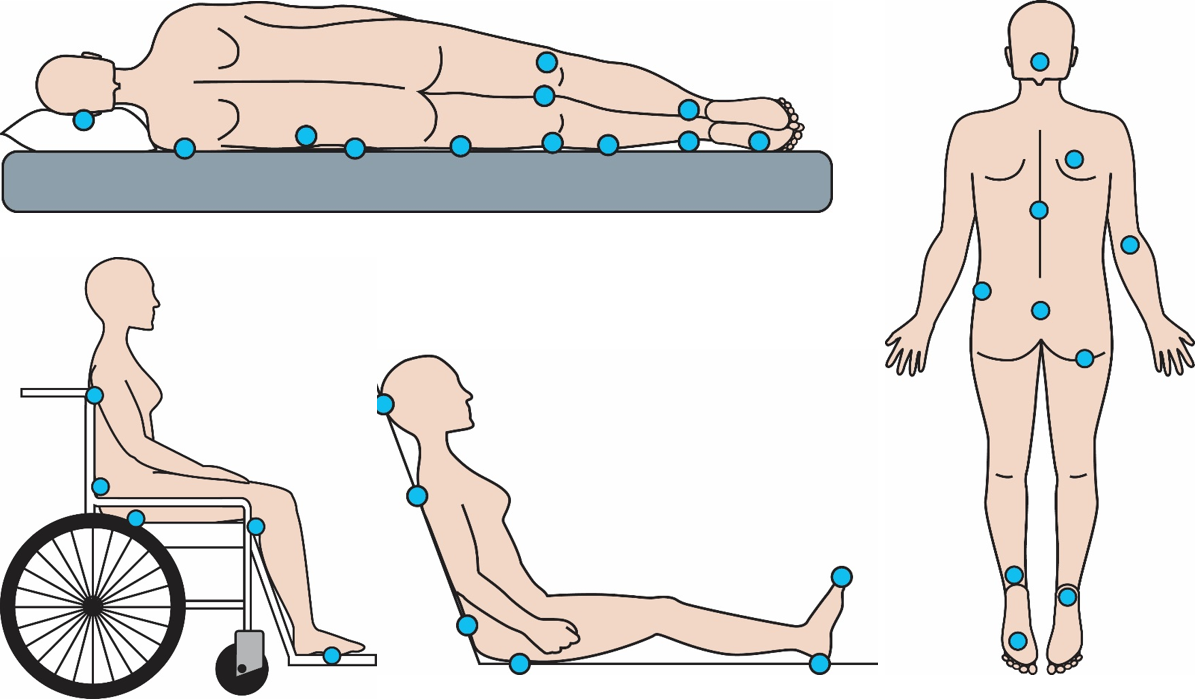
Common locations of pressure ulcers
Some of the areas most at risk include:
- back of the head
- shoulders
- base of the spine
- buttocks
- heels
- toes.
If you are at risk, check these areas regularly.
Early signs of a pressure ulcer
You may notice the following signs:
- change in the colour of your skin (red patches in light skin; bluish or purplish patches in dark skinned people) that does not go away
- change in the feel of your skin (soreness, pain, numbness)
- increased pain on any of the common locations (shown above)
- warm and/or hot sensation on any of the common locations (shown above)
- blistering of your pressure points
- swelling over the sore area of your skin
- grazes on the sore areas.
The signs to feel for are:
- patches of hard skin
- warm/cool pressure areas
- tenderness
- swelling especially over bony points.
Pressure relieving equipment
Do not use ring and/or doughnut cushions as these can cause further pressure damage.
If you are assessed as being at risk of developing a pressure ulcer, your healthcare professional will advise you on:
- the appropriate pressure relieving equipment for chairs and/or your bed
- how to use it effectively
- the limitations of the equipment.
Please be aware that using pressure relieving equipment is only part of the solution. Listen to the advice of your healthcare professional and discuss the best solutions for you.
Ways you can avoid pressure ulcers?
- Inform your healthcare professional if any areas are painful or sore.
- Change your position regularly if possible or ask for assistance to change your position.
- Avoid repeated friction and shearing. This can happen when you slide down or are moved up in a bed or chair.
- Support and elevate your heels to minimise pressure damage.
- Ensure you check your skin for signs of pressure damage at least daily or ask someone to do this for you (by looking in a mirror you may be able to see areas not normally visible to you).
- Do not rub your skin dry but pat gently.
- Protect your skin from moisture or dryness. Your healthcare professional and/or pharmacist can advise you on appropriate intervention and products.
- In warm or hot temperatures, try and keep cool and clean.
- Eat a well-balanced diet and drink plenty of fluids. Please seek advice from your healthcare professional if further information is needed.
- Try to reduce the number of layers between you and your pressure relieving mattress and/or cushion.
- Try to avoid crumbs or creases in the bed sheets and on chairs where you are sitting.
- Consider not smoking.
- Make sure the person helping you has read this leaflet.
Who should I contact if I am concerned?
If you think you may be developing a pressure ulcer please tell your healthcare professional or GP as soon as possible.
If we are treating your pressure ulcer and you have any concerns or questions about how it is healing please contact your Community Nursing Team.
This information should only be followed on the advice of a healthcare professional.
Do you have feedback about our health services?
0800 030 4550
Text 07899 903499
Monday to Friday, 8.30am to 4.30pm
kentchft.PALS@nhs.net
kentcht.nhs.uk/PALS
Patient Advice and Liaison Service (PALS)
Kent Community Health NHS Foundation Trust
Trinity House, 110-120 Upper Pemberton
Ashford
Kent
TN25 4AZ
![]()
Donate today, and help the NHS go above and beyond. Visit kentcht.nhs.uk/icare
If you need communication support or this information in another format, please ask a member of staff or contact us using the details above.
