Lung diseases
Last edited: 22/12/2022
This leaflet outlines a number of lung diseases. These diseases affect different areas of the lung. Some affect the larger airways – the trachea and the bronchi – and other diseases affect the small air sacs – the alveoli. The diagram illustrates the main airways and tissues of the lungs.

Chronic Obstructive Pulmonary Disease (COPD)
This is the most common lung disease. COPD encompasses three different diseases:
- Emphysema
- Chronic Bronchitis
- Chronic Asthma.
Chronic asthma
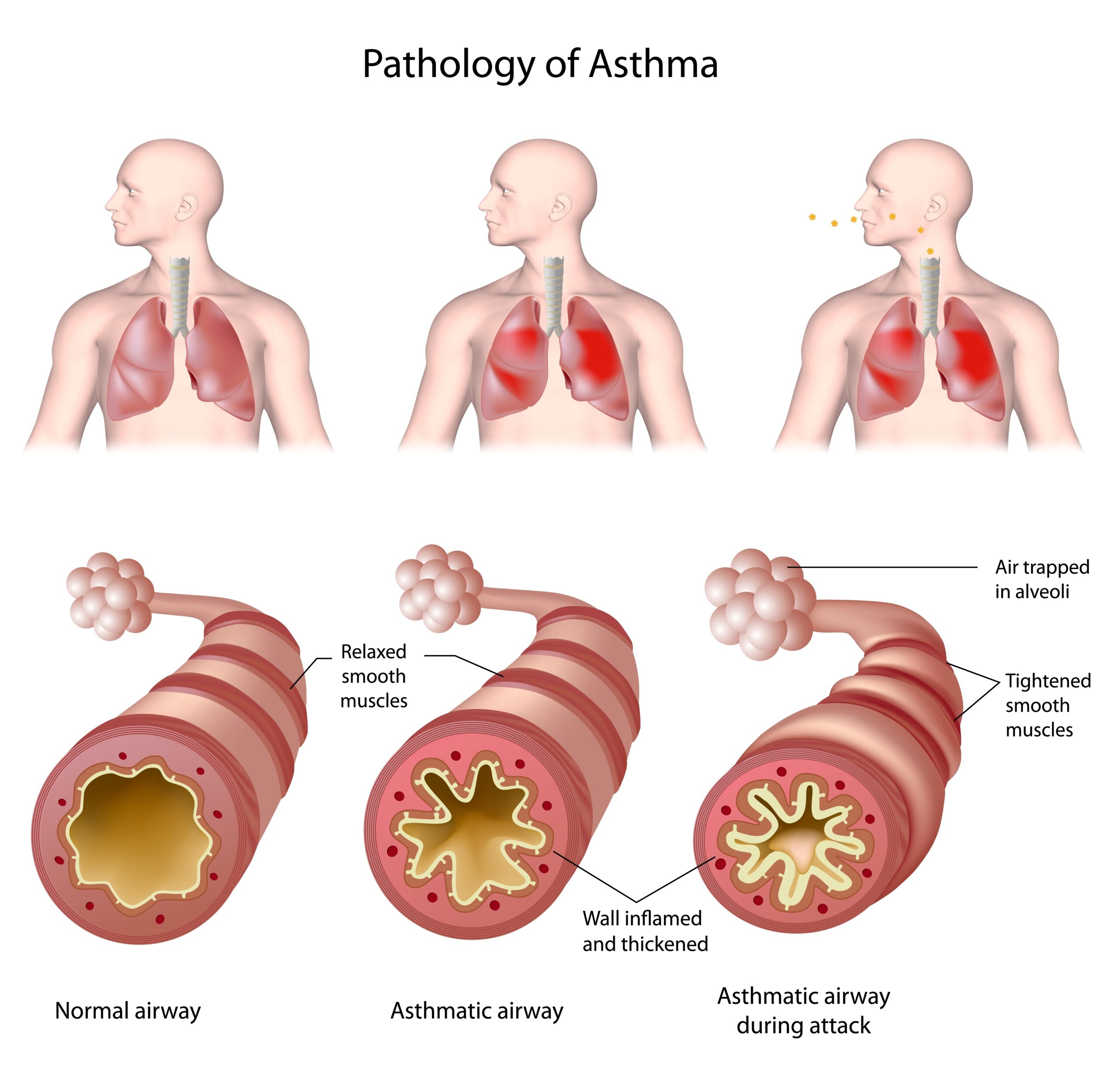
Asthma is a chronic inflammatory disease mainly affecting the larger airways – the trachea and the bronchi. Both the lining of the airway and the smooth muscle in the walls are affected.
The onset of asthma is usually sudden. If you suffer with asthma you will find that your airways are very sensitive and can quickly react to trigger factors such as dust or cold air.
The airways become narrow and sometimes produce more mucus than usual. This makes it difficult to breathe.
Symptoms:
- sudden onset
- allergy, eczema, hay fever, family history
- cough, especially at night
- chest tightness
- wheeze
- shortness of breath, often at rest.
Chronic Bronchitis
Bronchitis means inflammation of the bronchi. The bronchi are the airways which carry oxygen from the windpipe (trachea) into the lungs. The bronchi narrow progressively because of enlarged mucus producing cells which over-produce mucus and phlegm. The mucus wafting cells (cilia) are damaged and therefore phlegm cannot be dealt with by the body in the normal way, causing a chronic cough. Chronic Bronchitis is caused by pollutants and cigarette smoke.
Symptoms:
- chronic cough with copious amounts of phlegm, usually in the morning
- breathlessness on exertion.
A diagnosis is made if an individual has symptoms for three months, usually over the winter period, for two consecutive years.
Emphysema
This is a disease of the alveoli (air sacs) of the lungs. The alveoli lose their elasticity and cannot inflate and deflate as they used to. This then has an effect on the exchange of oxygen and carbon dioxide in the lungs. People who have emphysema have a reduced area of lung available for gas exchange and therefore become short of breath.
Symptoms:
- severe breathlessness
- over breathing
- pursed lip breathing.
Bronchiectasis
This is a disease that affects the bronchi. The bronchi contain tiny glands that produce a small amount of mucus. This mucus helps to keep your airways moist. It also traps the dust and germs that you breathe in. The mucus is usually wafted up to the back of the throat by the cilia (fine hairs) that line the airways.
In Bronchiectasis the airways are damaged leading to chronic inflammation, weakening and widening of the bronchi. The glands overproduce mucus, which begins to build up and cannot be effectively cleared by the cilia. Mucus begins to pool in the weakened bronchi, leading to infection. Recurrent infection and chronic inflammation leads to further damage.
There are several known causes including:
- an underlying genetic disease such as cystic fibrosis or primary ciliary dyskinesia.
- scarring of the lungs from previous damage (such as pneumonia, whopping cough or measles).
However, over half the people with Bronchiectasis in the UK have no obvious cause for it.
The most common symptom is coughing up phlegm, often in large amounts, every day. This is can be very tiring. Many people with Bronchiectasis also have wheezy shortness of breath and sinusitis.
Pulmonary Fibrosis or Fibrosing Alveolitis
This is a disease that affects the alveoli (small air sacs in the lungs).
Inflammation and repeated harm causes scarring and thickening of the alveoli, which reduces the amount of oxygen that can pass into the blood vessels from affected areas. The most common symptom is breathlessness. It is also common for people with fibrosis to have a drop in oxygen levels when they exert themselves.
A cough, which is often dry, is also common and finger clubbing, which is a change of shape of the fingernails may occur.
The cause of Pulmonary Fibrosis is still unknown. It is thought to be a result of over activity of the body’s immune system causing damage to the lungs.
The trigger for this self-damaging (auto-immune) process is not known, but may be multiple. It is often related to Rheumatoid Arthritis.
Treatment
- If you smoke, the single most effective intervention is to stop. Contact One You smokefree on 0300 123 1220 for help.
- Diet – eat a well-balanced diet.
- Exercise – is of vital importance to be incorporated into your lifestyle.
- Bronchodilators – there are different types of inhaled medication which work in different ways and can benefit symptoms.
- Individualised care plan – can help you manage your symptoms and reduce how often you may experience an exacerbation (known as flare ups).
- Flu vaccination – vaccination every autumn is worthwhile, as flu can cause exacerbations.
- Sputum clearance techniques – to keep your chest clear from mucus, particularly for conditions of Bronchiectasis and Bronchitis.
The Specialist Respiratory Team can provide education, advice and help to manage your condition.
References:
British Lung Foundation www.lunguk.org
British Thoracic Society www.brit-thoracic.org.uk
Contact us
Admin Team
Whitstable and Tankerton Hospital
01227 594657
kcht.pulmonaryrehab@nhs.net
Monday to Friday, 8am to 4pm.
This information should only be followed on the advice of a healthcare professional.
Do you have feedback about our health services?
0800 030 4550
Text 07899 903499
Monday to Friday, 8.30am to 4.30pm
kentchft.PALS@nhs.net
kentcht.nhs.uk/PALS
Patient Advice and Liaison Service (PALS)
Kent Community Health NHS Foundation Trust
Trinity House, 110-120 Upper Pemberton
Ashford
Kent
TN25 4AZ
![]()
Donate today, and help the NHS go above and beyond. Visit kentcht.nhs.uk/icare
If you need communication support or this information in another format, please ask a member of staff or contact us using the details above.
