Early post cardiac surgery care
Last edited: 16/12/2022
Lifting and domestic activities
Weeks one to six:
- Avoid any heavy lifting, pushing or pulling for the first six weeks.
- Do not lift more than a half full kettle in weight. Use both hands when lifting and keep the load close to your body.
- Do not walk a dog on a lead.
- Aim to do simple chores such as washing up, dusting, making tea, preparing simple meals and relaxing hobbies.
Weeks six to 12:
- Gradually increase the amount you can lift. Light bags of shopping, laundry and saucepans – not cast iron – and carry out light gardening.
- Walking a dog.
After 12 weeks:
- Build up to carrying heavier bags or saucepans, lifting young children, vacuuming, digging, mowing the lawn, playing golf, swimming, cycling and riding a motorbike.
- Your breastbone should be fully healed.
Sleeping
- You can sleep in whichever position you find comfortable.
- You may find you want an afternoon nap when you get home. This is okay but try not to stay in bed for too long as you may have difficulty sleeping at night.
Driving
- There is a legal requirement not to drive for four weeks after surgery but it is advisable not to drive for six weeks.
- Wear a seatbelt. You can make this more comfortable by using a small pillow or towel between your chest and the seatbelt.
- It is important that you let your insurance company know of your heart surgery, although this should not mean a change in policy. Not informing them may invalidate your insurance.
Returning to work
- Do not return to work before your follow-up appointment with your surgeon. The nature of your work should be considered.
- As a guide you should wait eight weeks for light work and 12 weeks for manual work.
- Have a gradual return to work where possible, with lighter duties or reduced hours.
Travel
- Do not take a long-haul flight for six to eight weeks after your surgery.
- If you go on holiday, remember to continue to pace yourself and to choose a holiday destination where there are good medical provisions, should you need them.
- Always make sure your travel insurance company is aware of any health matters. The British Heart Foundation has a list of sympathetic insurance companies.
Wound care
- You may be referred for ongoing wound care with your GP surgery or the Community Nursing Service.
- Keep it clean by having a wash or shower daily. Do not bath. Wash soap away thoroughly. Avoid using perfumed soap, creams or powders as these cause irritations.
- Scars may feel itchy, numb or tingly. This is a normal part of healing. Avoid scratching as it can introduce infection.
- If your wound becomes hypersensitive or tight, please speak to your physiotherapist for further advice.
- You might notice a notch or bump at the top of your chest wound. This is normal and will settle down after a few weeks.
- Some stitches may take weeks to dissolve.
- Leg wounds generally take longer to heal.
- Contact your GP surgery as soon as possible if you notice any of the following:
- red
- swollen
- hot
- very painful
- weeping or oozing yellow or green discharge.
TAVI wound care
- Normal for the groin to be tender for a few days and for a bruise to develop.
- Do not have a bath. You can shower but avoid rubbing the area.
- Do not put creams, powder or soap directly onto the groin site.
If you notice any of the following, please contact your GP:
- a hard-tender lump under the skin around area of incision – a pea size lump is normal
- increase in pain, swelling, redness and/or discharge at the site
- a cold foot on the same side
- a raised temperature or fever.
Pain management
- Effective pain control is essential to optimise recovery, allowing you to breathe, move and exercise more effectively and in greater comfort.
- Take your pain medication regularly and at the stated dose.
- If taking opiates such as codeine, reduce the dose and stop this medication first, whilst continuing with regular paracetamol.
- Drink plenty of plain fluids, particularly if you’re taking opiates as these commonly cause constipation.
- If constipated, contact your GP who may prescribe a laxative.
- If your pain is not well-controlled, contact your GP to discuss the options, such as alternative or additional pain medication.
Posture
- An awareness of your posture can aid recovery from surgery.
- The mid/upper back, neck and shoulders can get stiff leading to increased pain, altered posture and movement patterns.
- Aim to sit and stand as straight as possible with shoulders relaxed, back and down. Tuck your chin in keeping your gaze level.
- Check your posture before undertaking post-op mobility and breathing exercises.
- Use cushions and pillows to help you get comfortable.
- Avoid any movements or positions which increase pain.

Post-surgical neck and shoulder exercises
- Begin sitting up tall, unsupported.
- Tuck your chin in, keeping your neck and back straight – not tipping your head forwards. Hold at the end position and feel the stretch in your neck. Repeat five times.
- Tilt your head forward until you feel a stretch behind your neck. Hold for five to 10 seconds and bend your head backwards, as far as is comfortable. Hold for five to 10 seconds. Repeat five times.
- Tilt your head ear to shoulder. Hold for 10 seconds. Repeat on left and right sides, two times.
- Turn your head to look over your shoulder. Hold for ten seconds. Repeat on left and right sides, two times.
- Lift shoulder to ears then relax. Repeat five times.
- Circle shoulders forwards and backwards. Repeat five time in each direction.
- Clasp your hands together, slowly raise them in front of you, arms straight until you feel a comfortable stretch. Return to start and repeat five times. Increase range as this becomes easier.
- Sitting tall, squeeze your shoulder blades together to achieve a gentle stretch across the front of your chest. Hold for 10 seconds. Repeat five times.
- Reduce range of motion and/or number of repetitions if painful.
You can also find these instructions on our website, visit www.kentcht.nhs.uk/cardiac-rehab-programme/post-surgical-advice/post-surgery-exercises
Breathing exercises
Breathing exercises counteract the effects of anaesthetic. An altered breathing pattern reopens areas of collapse and regains full chest expansion.
- Sit up tall, shoulders back, down and relaxed. Take a long, slow, deep breath – try to keep your chest and shoulders relaxed. Breathe out relaxed and gently like a sigh. Repeat for three to five deep breaths. Some people find it beneficial to hold their breath for two to three seconds at the end of the breath in, before breathing out.
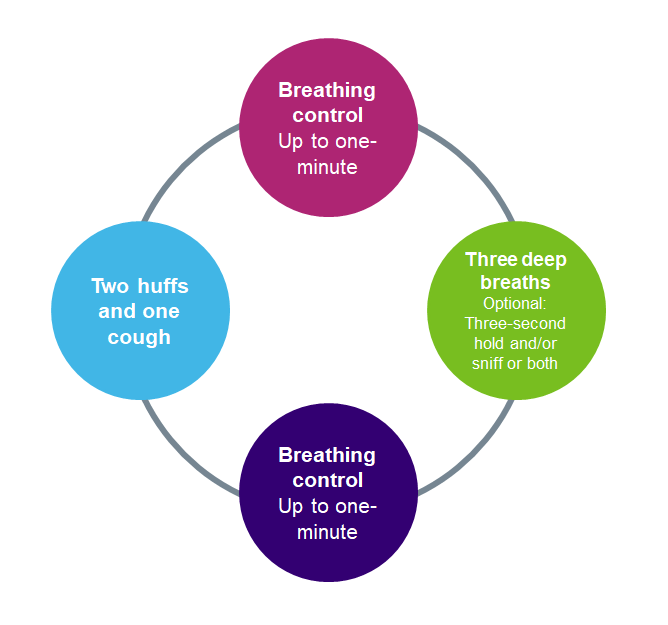
- The active cycle of breathing technique can be beneficial for secretion clearance.
- Support your chest with your hands or hug a pillow while coughing.
- Make sure you are well hydrated which will also help make secretions easier to clear.
Activity, rest and exercise
Walking is an ideal form of exercise. It will help optimise the benefits achieved by your surgery, as well as help you regain your cardiovascular fitness and return you to your everyday activities. It also helps to:
- improve constipation and circulation
- control blood pressure, weight and cholesterol
- improve strength, bone density, balance and co-ordination
- return to, or improve on, pre-operative activity levels.
Guidance for walking
- Aim to comfortably walk a moderate pace for 30 minutes, five days a week, six weeks after leaving hospital.
- Begin with the distance you were walking in hospital.
- Gradually increase the distance every two to three days.
- Use the neck and shoulder exercises as a warm-up and cool-down.
- Be aware that it will be more difficult if it is very cold, hot or windy.
Start each walk slowly and build up to a moderate pace. Finish by slowing back to a steady pace.
Do not:
- exercise for an hour after eating to avoid indigestion
- over exercise so you are exhausted at the end
- continue if you experience angina pain, nausea, dizziness, marked breathlessness or become cold and clammy – seek medical help if this happens.
Rest
- Make sure you get enough rest each day, especially following exercise.
- Do not be tempted to do too much, too soon.
- Pace yourself by spreading essential tasks evenly throughout the day and asking yourself if it needs to be done at all.
- Try and limit the number of visitors in the first few days as you can become tired very quickly.
- Be aware you will have good days and not so good days.
Endocarditis – information for valve patients only
Endocarditis is a rare condition. It is an infection of the inner lining, chambers and valves of the heart. Early diagnosis and treatment are important as endocarditis can damage your heart and be life-threatening. The symptoms of endocarditis can develop slowly over weeks or months or can develop suddenly.
The most common symptoms are:
- flu-like symptoms – these include having a temperature, tiredness, headaches, chills, a cough and sore throat
- unexplained weight loss
- pale skin
- aching muscles and joints.
You can lower your risk of developing endocarditis by:
- practicing good oral and dental hygiene
- visiting your dentist regularly
- avoiding body piercing or tattooing
- washing your hands regularly and properly to help stop bacteria spreading
- being aware of the symptoms and contacting your doctor if you are worried.
Further support
Please speak to your physiotherapist, nurse or the exercise and lifestyle team if you have any questions or concerns.
Contact us
Admin Team
0300 123 1709
kcht.communitycardiacrehab@nhs.net
Monday to Friday, 8.30am to 4.30pm
This information should only be followed on the advice of a healthcare professional.
Do you have feedback about our health services?
0800 030 4550
Text 07899 903499
Monday to Friday, 8.30am to 4.30pm
kentchft.PALS@nhs.net
kentcht.nhs.uk/PALS
Patient Advice and Liaison Service (PALS)
Kent Community Health NHS Foundation Trust
Trinity House, 110-120 Upper Pemberton
Ashford
Kent
TN25 4AZ
![]()
Donate today, and help the NHS go above and beyond. Visit kentcht.nhs.uk/icare
If you need communication support or this information in another format, please ask a member of staff or contact us using the details above.
