Dysfunctional breathing pattern
Last edited: 22/12/2022
Print this page
Share on social media
This content may not be reproduced, without the permission of Kent Community Health NHS Foundation Trust - contact us.
What is dysfunctional breathing?
Dysfunctional breathing is a term that relates to a change in your breathing pattern, from an efficient to a less efficient pattern.
It is to do with the mechanics of your breathing and does not always relate to a specific lung condition.
This change can feel sudden or can build up over time; there isn’t always an obvious trigger. Some of the common triggers include:
- anxiety or stress
- acute illness, for example chest infection or pneumonia
- long-term respiratory condition, for example COPD or asthma
- traumatic event – physical or emotional
- pain – especially in abdomen or lower back
- digestive issues, for example reflux or hiatus hernia.
If this change continues, your body can start to get used to this altered inefficient pattern without you even realising.
What is efficient breathing?
- Subconscious and automatic process.
- Effortless, relaxed and quiet.
- Nose breathing.
- Rhythmical, steady pattern (12 to 20 breaths per minute).
- Tummy movement.
- Breath in slightly shorter than the breath out.
- Able to talk in full sentences.
In normal breathing, 70 to 80 per cent of the work is done by the diaphragm (the main muscle of breathing which sits under the heart and lungs) and is the most energy-efficient and relaxing way to breathe.
What is inefficient breathing?
- Mouth breathing.
- Short, shallow breaths.
- Quick and erratic.
- Noisy.
- Raised shoulders.
- Movement at the top of the chest.
What are the common symptoms?
- Breathlessness.
- Persistent coughing.
- Excessive yawning or sighing.
- A feeling of not being able to take a deep breath.
You may also experience symptoms that do not seem to relate to your breathing including dizziness, poor concentration, pins and needles, bloating, fatigue and lethargy.
What can you do about it?
- Window breathing.
- Breathing control.
- Nose breathing.
- Understanding your triggers, for example managing anxiety, reflux or pain.
- Shoulder relaxation and postural correction.
- Continue to stay active.
You may be referred to a respiratory physiotherapist for further management.
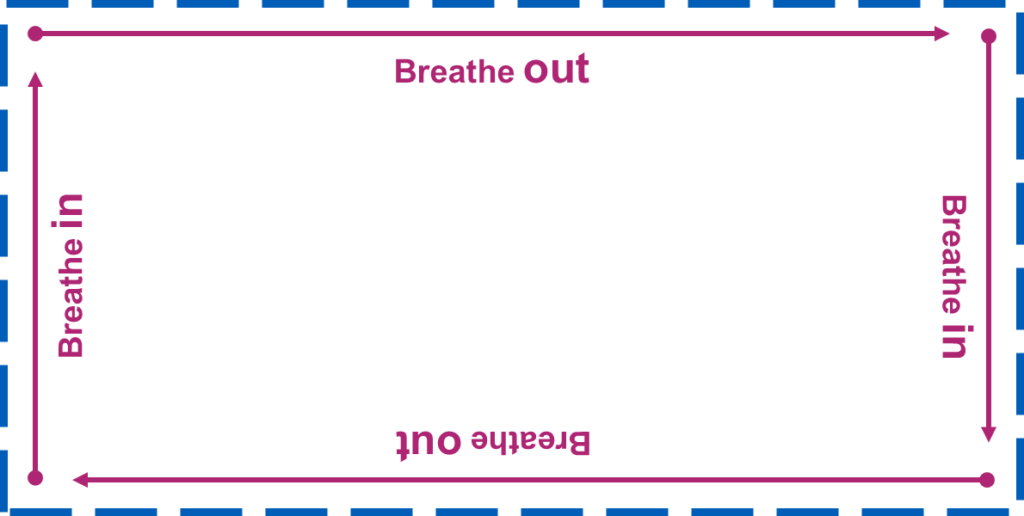
Window breathing
- Place your finger on the ‘dot’ in the top right of the rectangle.
- As you breathe in, follow the line in the direction of the arrow to the next corner.
- Breathe out along the next side.
- Continue around the rectangle following the instructions.
This breathing technique is helpful for getting your breathing into a more rhythmical pattern (breath in slightly shorter than your breath out). It is also very helpful as a distraction technique for when you have an episode of breathlessness or anxiety.
Breathing control (tummy breathing)
With a ‘normal’ breathing pattern you should see your tummy rising and falling as you breathe in and out.
Practicing your ‘tummy breathing’ can help to improve the effectiveness of your breathing and strengthen your diaphragm muscle.
- Find somewhere comfortable to sit.
- Either sit in a reclined or upright position, with your back well supported.
- Place a hand gently on your tummy just beneath your ribs. Don’t press too hard.
- Make sure your breathing is as steady and relaxed as possible.
- You should feel your hand rise as you breathe in and your hand lower as you breathe out – these are indications that your diaphragm is working properly.
Try and practice this exercise for three to four minutes, three to four times a day.
Don’t practice this when you are feeling very short of breath as you will find it difficult.
Importance of staying active
The symptoms associated with dysfunctional breathing can be debilitating both physically and emotionally.
Symptoms such as breathlessness, fatigue and anxiety can lead to inactivity and isolation.
This can lead to a cycle of inactivity:

Being active can help you to:
- breathe more efficiently
- improve your fitness levels and your tolerance to exercise
- improve your mood and emotional wellbeing
- improve your overall quality of life.
Breathlessness and activity
Breathlessness is a normal part of exerting ourselves. When we become more active, our muscles demand more oxygen from our lungs. This is achieved by:
- increased breathing rate
- larger breaths
- increased accessory muscle work (the muscles in your neck, upper chest and rib cage)
- increased movement in your upper chest.
However, if you are already breathing less efficiently (from your upper chest), you may already be using some of these mechanisms and therefore do not have the same reserves to draw upon.
This can lead to feelings of breathlessness that seem excessive for the amount of work you are doing.
It can therefore be difficult to know how hard you should push yourself during physical activity. The BORG Breathlessness Scale is a useful guide.
You should aim to be working at level three to four.
Remember this will be personal to you and may differ from somebody else’s idea of level three to four.
BORG breathlessness scale
|
Level |
Description |
|
0 |
Nothing at all: No breathlessness at all |
|
0.5 |
Just noticeable: Slight breathlessness but I can do this all day |
|
1 |
Very slight: Still more comfortable but breathing a little harder now |
|
2 |
Slight: Feeling good, getting a little warm but I can hold a conversation |
|
3 |
Moderate: Beginning to feel you’re working |
|
4 |
Somewhat difficult: I’m just above comfortable. A bit puffed and sweaty but still able to have a conversation |
|
5 |
Difficult: I can still talk but I’m definitely breathless and hot and sweaty |
|
6 |
Moderately severe: I can still talk but I don’t really want to. I am feeling very pushed |
|
7 |
Severe: Very breathlessness and struggling to keep going |
|
8 |
Very severe: I can grunt more than talk and can’t keep this pace up for long |
|
9 |
Very, very severe: Struggling to get m breath, unable to talk and need to stop soon |
|
10 |
Maximum effort: I can’t go any further, I’m ready to stop or pass out |
What can physiotherapy do?
- Increasing awareness and education about abnormal breathing patterns.
- Reassurance that things can improve.
- Learning how to use nose and mouth breathing in rest.
- Teaching about pacing and mobilising using nasal breathing.
- Breathing retraining in progressively taxing postures.
- Education about proper use for medications where applicable.
- Education about underlying respiratory diagnoses and how they affect your breathing pattern.
- Further recognition of triggers.
- Incorporating relaxation methods into everyday life.
- Control of symptoms during an episode.
- Manual therapy techniques.
- Encourage and support you in staying active or increasing activity levels.
Contact us
Admin Team
Whitstable and Tankerton Hospital
01227 594657
kcht.pulmonaryrehab@nhs.net
Monday to Friday, 8am to 4pm.
This information should only be followed on the advice of a healthcare professional.
Do you have feedback about our health services?
0800 030 4550
Text 07899 903499
Monday to Friday, 8.30am to 4.30pm
kentchft.PALS@nhs.net
kentcht.nhs.uk/PALS
Patient Advice and Liaison Service (PALS)
Kent Community Health NHS Foundation Trust
Trinity House, 110-120 Upper Pemberton
Ashford
Kent
TN25 4AZ
![]()
Donate today, and help the NHS go above and beyond. Visit kentcht.nhs.uk/icare
If you need communication support or this information in another format, please ask a member of staff or contact us using the details above.
